In July 2020, we predicted how healthcare environments and delivery would change in a post-pandemic world. While none of us knew exactly how long the pandemic would last or how it would evolve, even from its early onset, it was inevitable that the effects of the pandemic would impact the future of healthcare design. At the time, we anticipated:
- A contactless and more technologically dependent arrival sequence.
- Divided waiting rooms with smaller clusters of high-backed furniture.
- Exam rooms with a sterile, minimal aesthetic to convey cleanliness while featuring HEPA filters and touch-free control and devices.
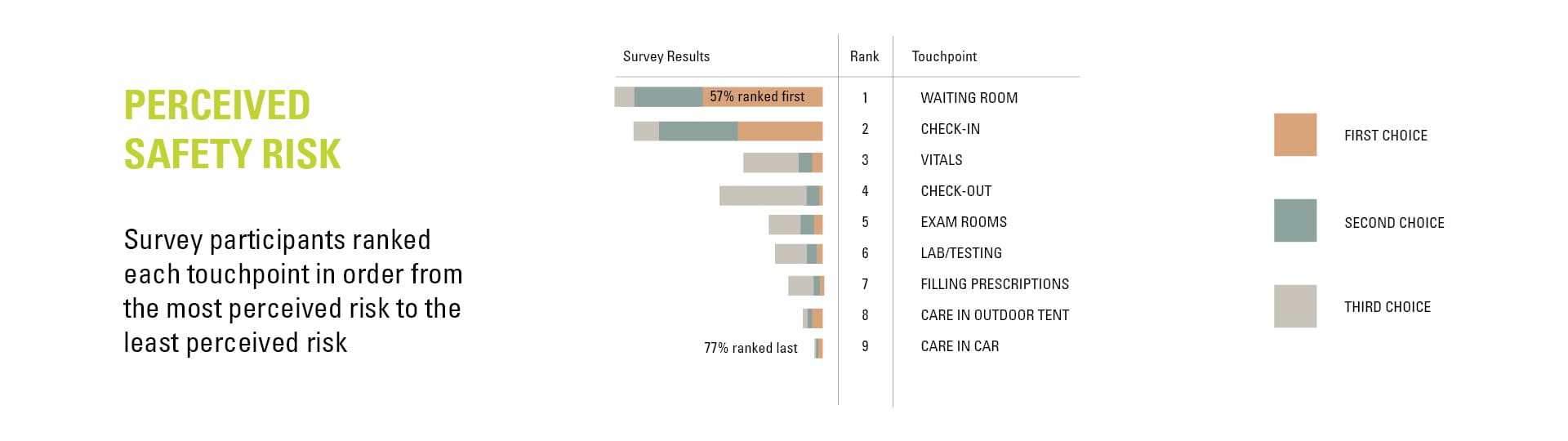
Around the same time as we made these predictions, we were asked by Atrium Health to propose design interventions that could help patients feel safer when visiting their facilities amidst the pandemic. This led to a one-month design sprint where we measured patients’ perceived levels of risk and proposed not only physical interventions but also practices and workflows that could ease the minds and spirits of patients and their families during the pandemic.
Three years later, we now see that we were on target with these predictions—but not necessarily in the ways we thought. Let’s look at two divergent ways people experience healthcare in a post-pandemic world.
Embracing Technology to Prioritize Convenience
We were right about the COVID-19 pandemic increasing the need to leverage technology. However, we didn’t realize just how much technology would be integrated into healthcare—way beyond a single aspect of the healthcare journey. As healthcare grows and evolves, telemedicine will continue to replace in-person care for a sizeable number of patients.
The rise of telemedicine
Virtual visits became commonplace during the pandemic thanks to a perfect storm of patients avoiding the physical doctor’s office (whether because they were obeying stay-at-home orders, quarantining, and/or simply being cautious about virus exposure), the CARES Act (which relaxed regulations on how telehealth could be delivered and reimbursed), and increased comfortability with video conferencing technology on the part of both providers and patients.
A national study showed that telemedicine encounters increased by 766% in the first three months of the pandemic.1
Most healthcare providers initially thought this surge in telemedicine use was just a stopgap to help meet the needs of patients during the height of the pandemic and would fade once COVID-19 became endemic. However, studies show that telemedicine has significant staying power.
Patients who use telemedicine like it, citing its ease of use, low cost, improved communication, and elimination of travel time as the reasons they might prefer it over face-to-face visits. Clinicians are a bit more varied in their opinions, with one-third stating that the overall quality of a visit is better in person.1 But, as the pandemic dragged on and acclimated us to the idea of remote work and technological tools, many doctors and support staff embraced telemedicine.
Does telemedicine address inequities in healthcare?
There was a widespread belief that the decreased barriers to telemedicine usage prompted by the pandemic could pave the way for significant progress in tackling inequities in healthcare access. However, data shows that in reality, “telemedicine favors individuals typically unburdened by the traditional care model, namely the young, white, and educated.”2 Yet, many are hopeful that with improved broadband access, public education about medical options, and adjustments to Medicare and Medicaid, telemedicine could do more to close the gap. More research needs to be done to confirm when telemedicine produces the best outcomes. For now, it seems more appropriate for chronic and less severe illnesses.
Telemedicine’s impact on design and construction.
A shift in healthcare delivery is anticipated, with many individuals opting for primary care through on-demand telemedicine services or retail stores. In this evolving landscape, hospitals will primarily cater to the most critically ill patients requiring in-person care.
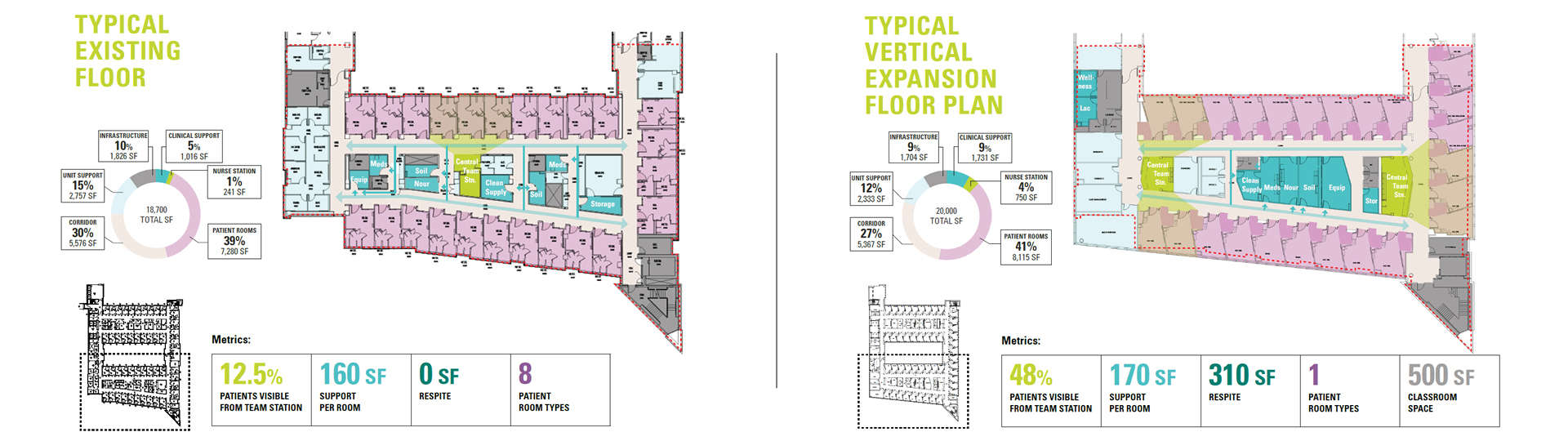
Spatial considerations for telemedicine will become pivotal, leading to the emergence of facilities or designated sections specifically tailored for virtual care. These spaces will demand meticulous attention to acoustics and technology integration. Moreover, the design of examination rooms will evolve to accommodate both in-person visits and telemedicine, embracing flexibility. Additionally, there is a likelihood that telemedicine consultations will be delegated to remote providers, resulting in the release of space previously reserved for individual provider offices.
Technology will also play a pivotal role in enhancing the in-person healthcare experience. Videoconferencing technology allows families to stay connected with their loved ones in the hospital, even if they step away to grab a snack. Additionally, it serves as a valuable tool to include family members in discussions about the outcomes of in-person visits, ensuring that pertinent information is communicated and shared in a timely and accessible manner.
The Human Touch: Doubling Down on People-Focused Care
We were correct in anticipating that the COVID-19 pandemic would result in healthcare settings offering more designated spaces for staff respite. Yet, we might have underestimated the extent to which it would emphasize the crucial need for both staff and patients to experience compassion in spaces that exude warmth and human connection.

At the opposite end of the spectrum from what could be considered the impersonal, cold, convenience-oriented world of telemedicine is a newfound appreciation for the people at the center of healthcare interactions. The pandemic was a “hands off” time in healthcare when PPE prevented patients from seeing their doctor’s face, families and visitors couldn’t visit their loved ones in the hospital, and overworked healthcare staff didn’t have time or space to process the death and fear they faced on an hourly basis.
Pre-pandemic, it was a challenge to convince some of our clients that even a small lactation room for nursing mothers on their staff was a necessary amenity in their projects. On one of our projects, we got a wellness room into the program, only to visit months later and find that it had been converted into an office. It is typical to tour existing facilities where our plans indicate a “staff lounge” only to find it jam-packed with workstations or supplies. When space is at a premium, amenities for staff—and even patients—are the first to go.
The COVID-19 pandemic publicized the plight of overworked essential hospital workers, which helped dramatically shift the attitude about staff amenities. Lounges and respite spaces that were once considered luxuries used to attract top talent are now considered necessities that acknowledge the humanity of healthcare workers and alleviate some of the extreme stress of their jobs. On the patient side, there seems to be an even greater desire for spaces that encourage a calmer mental state, ample space for families and visitors, and a less tech-heavy, more personal, and human-centered experience.

